,
by Sharon Reynolds
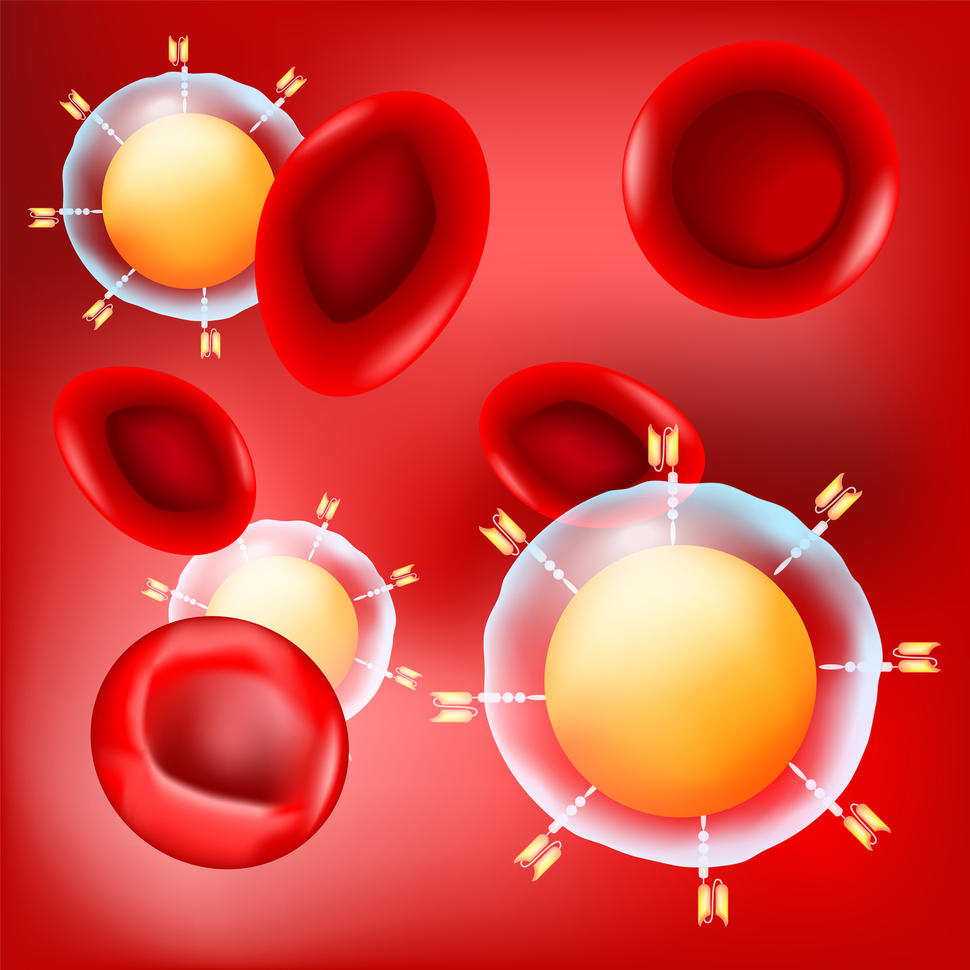
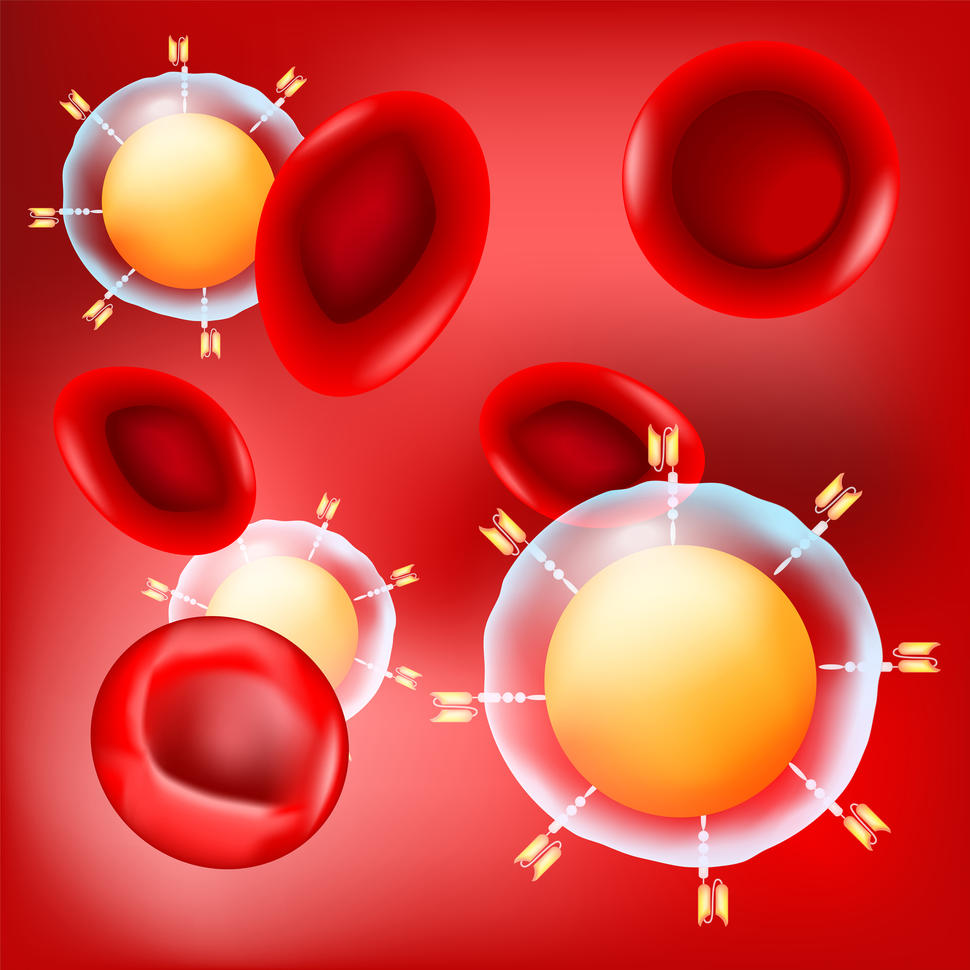
For some folks with blood cancers like leukemia and lymphoma, CAR T-cell therapies have confirmed to be a transformative remedy. However for strong tumors like breast, colorectal, or pancreatic most cancers, which make up about 90% of most cancers circumstances, success with T-cell therapies has been more durable to come back by.
One large purpose for these failures is that T cells, the immune system’s main protection in opposition to contaminated and diseased cells, typically turn out to be weakened and incapacitated within the poisonous surroundings discovered inside and round strong tumors. Researchers have been exploring some ways to assist CAR T cells and different experimental T-cell therapies survive inside these hostile environment, often called the tumor microenvironment.
In a brand new examine, an NCI-funded analysis group confirmed the promise of 1 such tactic: seeking to the genetic modifications that cancerous T cells themselves use to remain alive and develop. Incorporating these genetic modifications into T-cell therapies, the group discovered, might make them higher most cancers killers.
When examined in mice, T cells engineered to have one particular genetic alteration the group found in cancerous T cells gave the engineered cells “superpowers,” mentioned Jaehyuk Choi, M.D., Ph.D., of Northwestern College, who co-led the examine.
Including the genetic change, a fusion of elements of two genes, helped the engineered T cells divide quicker, kill extra tumor cells, and survive for greater than a yr within the handled mice. And, importantly, it didn’t make the T cells behave like most cancers cells, the researchers reported February 7 in Nature.
“Once we added [this] single mutation, we didn’t see the kind of unrestrained [T-cell] development [you see in cancer], nevertheless it gave [the engineered] T cells capabilities that they don’t naturally have,” defined the examine’s different chief, Kole Roybal, Ph.D., of the College of California San Francisco.
The primary twenty years of T-cell remedy analysis centered on the fundamentals, defined Rosa Nguyen, M.D., Ph.D., who research mobile therapies in NCI’s Middle for Most cancers Analysis however was not concerned on this examine. That work included determining what molecules on most cancers cells could be focused by T cells and find out how to change T cells to higher establish such targets, as is completed in CAR T-cell therapies.
“Now individuals are getting tremendous artistic in developing with various things [to add] to those cells to make them work higher,” Dr. Nguyen mentioned. “That’s what the sector is transferring towards now.”
Harnessing nature’s survival methods
Any sort of cell within the physique has the potential to show cancerous, even immune cells. As its identify implies, the blood most cancers referred to as T-cell lymphoma begins in T cells.
These cancerous T cells have one thing many regular T cells typically lack: the flexibility to thrive within the hostile surroundings of a tumor. That surroundings can embrace different immune cells that truly work to decelerate or disable T cells, in addition to different cells and molecules that make it laborious for T cells to operate.
Dr. Choi’s lab has been finding out the survival traits of T-cell lymphomas for over a decade. “It’s … superb how these T-cell cancers have developed methods to guard themselves,” he defined.
From the angle of growing a T cell–based mostly remedy, lots of the mutations present in cancerous T cells present a further benefit, Dr. Choi defined: Any one among them, by itself, isn’t more likely to direct a cell to turn out to be cancerous.
Their years of analysis clearly confirmed that “nature has already achieved this large experiment to make [cancerous] T cells stronger,” he defined. So “we thought possibly [nature] can present us the way in which” to enhance T-cell therapies.
Higher, faster-acting, and secure T cells
Becoming a member of forces with Dr. Roybal’s lab, which makes a speciality of T-cell engineering, the researchers first rigorously analyzed a variety of cancerous T cells from T-cell lymphomas, in search of genetic alterations that appeared to assist them survive in that tumor microenvironment.
They initially discovered 71 candidate alterations. In additional laboratory experiments, they engineered CAR T cells to have a number of the most promising candidate alterations, and this achieved what the researchers had hoped: They elevated the CAR T cells’ potential to kill most cancers cells and preserve creating extra CAR T cells.
Further work revealed what seemed to be essentially the most promising alteration: a fusion of elements of two genes, CARD11 and PIK3R3.
“This single [fusion] activated many issues that folks have predicted would assist [improve] T-cell therapies,” Dr. Choi defined. In experiments in mice, treating them with CAR T cells engineered to specific this fusion gene elevated the manufacturing of molecules that T cells have to survive and performance.
And these enhancements solely occurred when the particular protein acknowledged by the T cells’ specialised receptor, their chimeric antigen receptor, was current. That’s, these extra-engineered CAR T cells would solely turn out to be supercharged the place and when wanted inside a tumor.
Improved T cell survival and persistence in strong tumors
The group examined the CAR T cells engineered to specific the gene fusion in mouse fashions of various cancers, together with strong tumors like mesothelioma and melanoma. Throughout these experiments, they discovered that the remedy was far more efficient at shrinking tumors—and protecting them below management for longer—than CAR T cells with out the fusion.
“Persistence, the flexibility to stay round within the tumor microenvironment, is the most important drawback [these cells] solved,” Dr. Choi mentioned. Whereas T cells with out the fusion died inside a number of days, those with the fusion “appear to stay round for so long as wanted,” he mentioned.
The remedy was very efficient regardless that the mice didn’t additionally get chemotherapy, Dr. Choi identified. That’s necessary as a result of presently, “virtually everybody who will get handled with [T-cell therapies] must have what’s referred to as conditioning chemotherapy beforehand,” Dr. Choi defined. However this chemotherapy could cause unintended effects, typically extreme sufficient that sufferers have to attend longer to get the T-cell remedy or presumably stopping them from doing so in any respect.
“If we ever need these kinds of therapies to be given in much less specialised facilities, and even within the outpatient setting, we have to do away with these cumbersome methods [like conditioning chemotherapy] which might be poisonous to sufferers,” added Dr. Roybal.
The researchers additionally engineered the fusion into a special sort of T cell–based mostly immunotherapy, referred to as TCRs, and noticed related outcomes.
In a mouse mannequin of melanoma, for instance, TCR T cells with the fusion gene flowed into tumors in a lot higher numbers and killed tumor cells far more successfully than TCR T cells with out the fusion gene. The TCR T cells with the fusion even confirmed this benefit at beginning doses 20 to 100 instances decrease than TCR T cells with out the fusion.
Having the ability to give a decrease dose of a T-cell remedy would supply one other security benefit for sufferers, Dr. Roybal defined. Present CAR T-cell therapies, that are given in giant doses, have the potential to trigger a harmful—and even deadly—immune system overreaction referred to as cytokine launch syndrome. That danger would possible be decrease with a smaller dose that ramps up its exercise over time, he added.
The researchers additionally tracked the T cells within the mice for greater than 400 days after remedy. Although they initially multiplied quickly to kill the tumors, their numbers then shrank again down and confirmed no indicators of changing into cancerous themselves.
Testing supercharged T cells in folks
The researchers have launched a biotechnology startup to maneuver their CAR T-cell remedy with this gene fusion into human trials, though they’re possible 2 to three years away from launching these research, Dr. Roybal defined.
Finally, researchers might need to attempt mixing and matching alternative ways to soup up T cells, Dr. Nguyen mentioned. However these approaches first should be examined one after the other to higher perceive how each works. “Now we have to make use of a stepwise method,” she mentioned.
Drs. Roybal and Choi additionally need to preserve exploring the handfuls of different promising mutations their display initially uncovered.
“We discovered lots of completely different mutations … that would [potentially] be used” in T-cell therapies to deal with “a wide range of several types of most cancers,” mentioned Dr. Roybal.
“Possibly the [CARD11–PIK3R3] fusion protein might be good for [fighting] some subset of strong cancers. And one of many different [mutations] we discovered might be necessary for an additional subset,” he mentioned. “That is the start [of this research], not the tip.”